View a PDF version of these comments here.
The Honorable Chiquita Brooks-LaSure
Administrator
Centers for Medicare & Medicaid Services
U.S. Department of Health and Human Services
Re: Proposed Collection and Comment Request - Requirements Related to Surprise Billing; Part II (CMS-10791)
Dear Administrator Brooks-LaSure:
On behalf of our 25,000 physician, resident, and medical student members, the Massachusetts Medical Society (MMS) appreciates the opportunity to provide comments in response to the Centers for Medicare & Medicaid Services (CMS) Proposed Collection and
Comment Request on Requirements Related to Surprise Billing; Part II (CMS-10791). In particular, we appreciate the opportunity to provide feedback on health care provider burden as it relates to the Good Faith Estimate (GFE) and Patient-Provider Dispute
Resolution Process requirements under the No Surprises Act (NSA).
The MMS has long held the position that patients should be protected and held harmless from surprise medical bills, and we have supported measures to increase price transparency in health care. The MMS was closely involved with our Congressional leaders
working to draft the No Surprises Act, and we appreciated that the resulting bill aimed to protect patients, while taking into consideration the concerns of physicians and hospitals. We appreciate that implementing regulations also include strong
patient protections and price transparency measures.
However, we are concerned that certain provisions, like the GFE and Patient-Provider Dispute Resolution Process, could have unintended consequences, undermining patient access to care and creating unnecessary confusion and burden when interacting with
existing state laws. We urge the agencies to consider the below feedback for future rulemaking. In addition, we support the recommendations made by the American Medical Association (AMA) enclosed with these comments.
Provider Burden Considering Health Care Workforce Challenges
Provider burden from the good faith estimate is increasingly of concern, given the workforce shortages and other challenges plaguing the health care system.
For example, the COVID-19 pandemic has created significant financial challenges for physician practices that will persist for years. During the pandemic, many physician practices and health care facilities have seen large decreases in patient visits due
to a combination of executive orders and patient fear about their safety and exposure to the COVID-19 virus. Massachusetts again had to curtail elective procedures during the Omicron COVID-19 surge. Increasingly, physician practices are having to
make tough decisions on whether they will be able to sustain their practices and stay open after the pandemic. For example, a survey by Harvard Medical School and developed through a partnership of clinicians, researchers, and public and private entities
in Massachusetts found that 20-40% of practices reported consolidating, selling, or closing their practice in 2020 (this statistic was driven mostly by independent practices, including primary care).
In addition to the challenges created by the pandemic, ongoing, systemic workforce challenges are also affecting physician practices, increasing the cost and effort to maintain an adequate clinical and office staff. For example, it is difficult for physician
offices to recruit and retain staff, since many front office staff, medical assistants, registered nurses, or technicians are finding jobs elsewhere (often outside of the health care sector) that have lower health risk or less stress. Specialty practices
such as radiology clinics have had significant challenges recruiting technical personnel necessary for mammograms and colonoscopies. In these critical preventive services, there are sufficient imaging machines and enough physicians to perform and
read the tests but without enough supplementary medical professionals, significant limitations on services lead to longer wait times for patients, which ultimately leads to delayed diagnoses and poorer health outcomes. Physicians in Massachusetts
are having to shorten the hours that they see patients due to not having adequate staff, cutting hours in the evenings or early mornings, which has the greatest impact on the most underserved populations.
These workforce shortages lead to physician practices being understaffed, resulting in less coordination of care with a negative impact on patients and the quality of their health care experience. It threatens to push providers towards employment by hospitals
or larger health systems (instead of smaller practices), which generally yield lower volume of care and higher cost—and issues with patient access to quality care as a result. Therefore, these ongoing workforce challenges, coupled with increased administrative
burdens on providers, further threatens physicians’ ability to sustain their practices and continue to deliver care to their patients—and will undoubtedly undermine patients’ access to care.
Provider Burden Concerns as a Result of the Good Faith Estimate (GFE)
As outlined in the Requirements Related to Surprise Billing, Part II rulemaking, the GFE is a notification of expected charges for a scheduled or requested service, including those that are reasonably expected to be provided in conjunction with the care,
and it is considered part of medical record. When scheduling care, or upon request, a provider must determine if a patient has and is planning to use health insurance coverage.
If the patient has health insurance coverage, the provider will send the GFE to the plan to generate an Advanced Explanation of Benefits (AEOB). This part of the rule has not been implemented. Overall, we appreciate that the implementation of the GFE
requirements related to the AEOB for insured patients was delayed. The delay will provide additional time to work with our members and other stakeholders in the physician community to best advise CMS on the implementation of this portion of the rule.
The extra time will also help ensure that solutions for implementation do not create additional cost and waste in the healthcare system, while ensuring our patients receive meaningful price information prior to their care. We hope the comments described
in this document on health care provider burden offer helpful information to the CMS in preparing future rulemaking on the AEOB.
Currently in effect, however, is the process by which a GFE is to be provided to patients who are uninsured or self-pay. If the patient is uninsured or self-pay, a GFE will be prepared by the provider and be provided directly to the patient. The MMS has serious concerns about the burden placed on providers due to the GFE process, especially the burden on the convening provider and the impact these burdens will have on physician practices as these requirements are enforced.
Below, we detail specific areas of concern and potential recommendations to reduce or prevent further administrative burden for health care providers:
- Additional Burden and Cost due to Broad Definitions and Scope
Notably, the IFR establishes definitions that are broader in scope for “provider” and “facility” than other sections of the No Surprises Act and related rulemaking. In
particular, these provisions apply to a wide range of providers and health care facilities, including small, independent physician practices (many of those outside of typical “surprise billing” scenarios) and safety net providers (like community
health centers who may treat a higher proportion of uninsured patients). Moreover, extra burden is placed on the “convening” provider or facility to provide the GFE. The MMS has concerns about the broad application of this provision. This will
place undue administrative burden on providers, particularly those smaller, independent practices or safety net providers that do not have extensive resources to track down and develop the required information for the GFE—or hire additional staff
to do so.
Furthermore, per the rule, the provider must inform a patient when scheduling that they have the right to request a GFE; however, the rule also suggests that any conversation about costs is meant to trigger a GFE. This means that
a patient may request a GFE to compare costs and make a decision about from where they will seek care, or whether they will submit a claim to insurance or self-pay. (These individuals would be considered self-pay for purposes of the requirement
on the provider or facility to provide a GFE.)
The MMS supports patients receiving meaningful and actionable cost information before their care, but we have concerns about unintended consequences. For example, because any conversation about
costs triggers a GFE, it could mean that some patients receive GFEs when they did not want them or prefer to use other price transparency tools offered by the provider. There is no automated way to make requests and communicate costs between convening
and co-providers, so this will lead to providers investing significant time and resources developing GFEs for patients they may not see. It is important to consider that the definitions and scope of this section of the rule may add additional cost, burden, and waste to the health care system. As CMS works to develop the requirements for the GFE as part of the Advanced Explanation of Benefits (AEOB), we urge the department to consider narrowing the definition and scope for providers required to provide a GFE (to insurers for generating
the AEOB) to only those in typical “surprise billing” scenarios (i.e., non-participating provider at a participating facility). We also encourage CMS to consider developing an automated and standardized electronic tool for providers to transmit cost estimate requests and information to other providers and to insurers (for the AEOB). Without this tool, providers will likely develop their own manual workflows that will lead to inconsistency in information, causing further administrative burden.
- Burden on Convening Providers; Managing Co-provider Information
As mentioned above, the convening provider or facility is responsible for determining if the patient is uninsured or self-pay, must notify the patient that a GFE is available
upon scheduling, and will provide the GFE to the uninsured or self-pay patient. As part of developing the GFE, the convening provider or facility is responsible for contacting all applicable co-providers and co-facilitators no later than 1 business
day after the request for the GFE is received (or the primary item or service is scheduled). The convening provider or facility is also responsible for requesting submission of expected charges from all applicable co-providers and co-facilities.
The MMS is concerned about the time and resources that will be required and the administrative burden placed on convening providers needing to track down information from co-providers. Furthermore, there is no easy, automated process to allow a provider to determine who the co-providers will be when scheduling care—nor is there an easy way to contact those providers for a cost estimate. With no automated process, this will cause disruptions to staff workflows and put enormous pressure on staff time and resources tracking down this information. This requirement has the potential to force providers into hiring staff to primarily
create GFEs for patients, which could be a challenge due to the workforce shortages mentioned above.
Additional clarity is needed on what happens when a co-provider is delayed in providing cost information to the convening provider
or when the convening provider is unable to determine within the deadlines who the co-providers will be. We appreciate that previous rulemaking acknowledged the potential challenges of providing GFEs in the IFR, particularly in situations involving
co-providers or co-facilities. The enforcement discretion provided in the rule will certainly help providers adjust to the new policies; however, we urge the department to recognize in enforcement decisions when providers have made a reasonable
attempt to provide the necessary information to patients.
- Concerns with Provider Access to Required Information
The GFE must include several elements, including:
- Patient name/date of birth;
- Description of the service and the date primary services are scheduled;
- Itemized list of services, grouped by provider or facility, reasonably expected to be provided—including those in conjunction with the primary services for that period of care;
- Applicable diagnosis codes, service codes, and charges associated with each service;
- Name, NPI, and TIN of each provider and states and facility location where care will be provided;
- List of services that the convening provider/facility anticipates will require separate scheduling;
- Disclaimer that there may be additional services that the convening provider/facility recommends as part of the course of care that must be scheduled separately and not reflected;
- Disclaimer that the information is only an estimate;
- Disclaimer that informs patient about the right to initiate the dispute resolution process; and
- Disclaimer that the GFE is not a contract.
As highlighted above, the GFE must include a wide range of information, and the MMS is concerned that some of that information may not be readily available to the convening provider—and trying to track it down will cause significant, additional
burden. It is unreasonable to require convening providers to provide information that they do not easily have access to or would have difficulty obtaining. For example, it will be difficult for providers to obtain the NPI or TIN for co-facilities
or accurate diagnosis and service codes for outside facilities or ancillary providers. Furthermore, a convening provider may not know what other co-providers will be providing services (like radiology, pathology, or anesthesiology) at the time
of scheduling. They may also likely not be able to determine at the time of scheduling what specific services are required to know what co-providers may be involved. A surgeon, for example, can expect to use services like anesthesia and radiology
at a hospital or other facility, but likely won’t know which individuals will provide those services when the GFE is developed. There are also challenges with the predictability of information prior to care as issues arise while a patient is being
treated. Medical needs often become apparent during a physician visit, especially for primary care. During the course of a visit, a provider may identify a need for (and perform) unforeseen services not included in the GFE, like non-routine labs.
This could be a significant difference in charges from the initial GFE—and updating the GFE with each change in treatment will cause additional burden.
This makes it extremely difficult for the convening provider to prepare an accurate
GFE when several other co-facilities or co-providers are involved in the item or service. Therefore, we urge CMS to consider amending the rule to limit the information that convening providers are required to provide from the co-facilities and
co-providers. One solution to help ease burden would be to only require convening providers to provide a list of the additional services patients can expect in conjunction with the primary service.
- Timing Concerns
The convening provider or convening facility is responsible for providing the GFE to uninsured (or self-pay) patient within 3 business days upon request. Information on scheduled care must be furnished within 1 business
day of scheduling care that is to be provided in 3 business days; and within 3 business days of scheduling care to be provided in at least 10 business days. When a GFE is provided initially in response to a request and then the item or service
is subsequently scheduled, a new GFE must be provided to the uninsured (or self-pay) individual under the established timelines.
The MMS understands that this timeline was established in the No Surprises Act and CMS has limited
flexibility in changing the timeline. However, it is important to note that this timeline is very difficult for convening providers to meet (particularly without an automated tool or standardized method to rapidly generate a GFE). This
is especially challenging given the ongoing workforce challenges threatening the sustainability of physician practices. As mentioned above, workforce shortages are increasing the cost and effort to maintain an adequate clinical and office staff,
and physician offices are struggling to keep up with their day-to-day responsibilities. The added administrative burden created by confusing and challenging timelines in this rule could be incredibly problematic for physician practices.
We are concerned that the timeframes outlined in this section may have the impact of delaying care. Providers may need to push back scheduled care to meet the timelines required to send a GFE to the patient. The timeline is also confusing, as
it conflicts with the timeline established in earlier rulemaking for the notice and consent provisions, which also require a GFE. We are worried these two sets of conflicting timelines will confuse providers and lead to additional administrative
burden. We urge CMS to develop and make available additional educational materials and trainings for physicians and other providers on these requirements.
- Confusion and Burden of Overlapping State and Federal Price Transparency Laws
There is also significant burden with the GFE provisions when considering how they interact with related state laws. Other provisions in the rule preempt state
law, but that is not the case for the GFE provisions.
For example, a Massachusetts notice and price transparency law is set to be implemented on July 31, 2022, and it requires similar information be shared with the patient as the GFE
requirements of the NSA. However, the underlying definitions used to determine which types of providers the law applies to, and the types of patients required to receive the price transparency information, is fundamentally different between the
state and federal laws. An example of the difference in definitions is that the federal NSA GFE provisions apply to patients who are uninsured or self-pay—defined as not having benefits or deciding not to use their benefits for an item or service.
The state law, however, uses the definition of whether a patient is out-of-network or in-network. This creates a situation where providers in Massachusetts may need to provide several, separate forms with the same or similar information to patients.
In fact, there are some scenarios (for example, if a patient has a PPO plan where a provider is out of network but a patient is “insured” in that they do have some out-of-network benefits for an item or service, but have decided to do self-pay)
where a provider could need to provide the state-required information, the federal information, and potentially also the separate federal notice and consent requirements (if a nonparticipating provider at a participating facility). A provider
in Massachusetts may have to provide potentially three new, different documents to the patient—all with similar price transparency information, but in different formats. This is not only a huge burden to prepare these new documents and ensure
each meets the requirements of the law—but this is also extremely confusing for patients receiving multiple documents.
To add on to the confusion for providers and patients, the state law differs greatly in the timeline required to
share this information. The state and federal laws also have differing requirements on what information needs to be shared with the patient, as well as the format in which to share that information. There are also stringent, but distinct, penalties
placed on providers who do not comply with the state and federal timelines. For example, if a provider follows the process and timeline as outlined in the federal NSA, they run the risk of missing state-required deadlines and could face penalties
of up to $2,500 for each instance of non-compliance. But if they act in good faith and follow the requirements set forth in the state law, they could face penalties of up to $10,000 for each instance of non-compliance with the federal law.
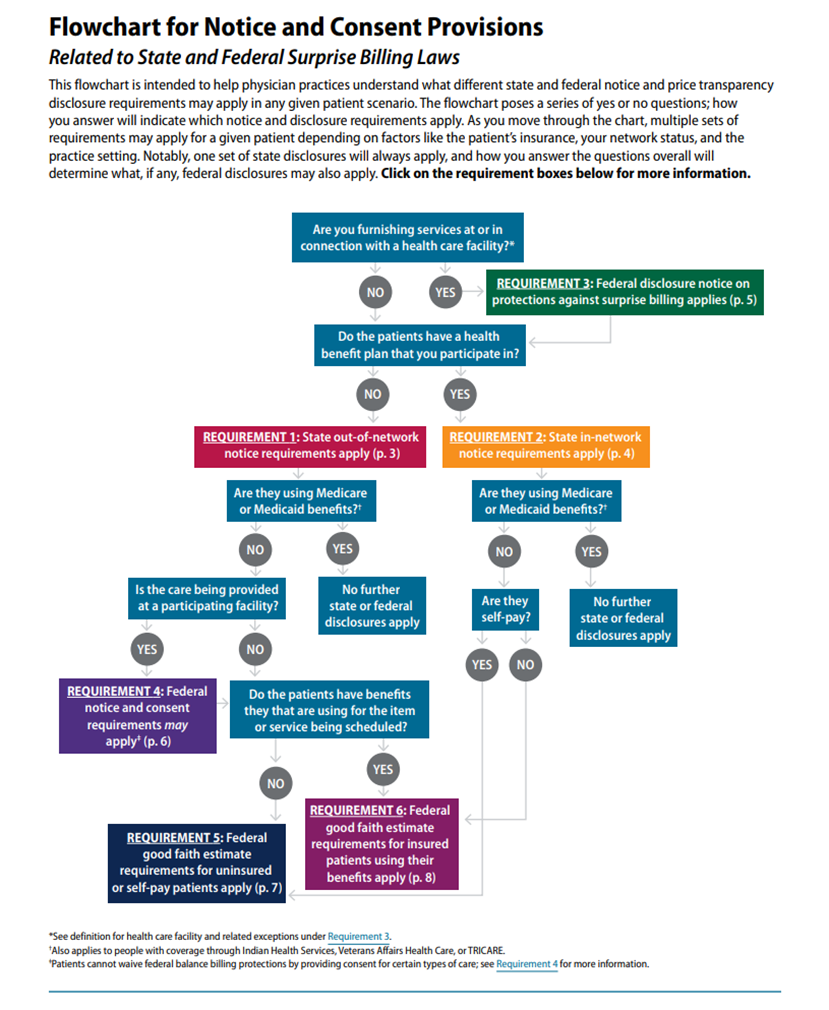
As alluded above, what results from the two, overlapping sets of laws is an extremely confusing web of requirements. This has created significant confusion for providers in Massachusetts trying to understand their requirements to comply with both
the state and federal laws at the same time. In fact, the Massachusetts Medical Society spent significant staff resources to map out a flow chart to help determine when each law applies, along with the necessary requirements (see image in Appendix
A below). As demonstrated in the flow chart, it is very complicated to understand how the two laws interact. Health care providers—especially small, independent physician offices—do not have the resources and background to properly understand
these confusing requirements. They may likely need to hire additional staff or external consultants to manage price transparency requirement workflows.
Therefore, we are extremely concerned about the administrative burden our Massachusetts providers are now facing when trying to reconcile the two competing laws and the financial cost if a provider (in good faith) follows the federal timeline over the state timeline (or vice versa). The MMS urges CMS to consider overlapping state GFE laws in future rulemaking, particularly as the they prepare plans for the GFE as part of the Advanced Explanation of Benefits (AEOB). The MMS also urges CMS to provide additional clarity on whether the requirements outlined in Requirements Related to Surprise Billing Part II are intended to preempt state law, as this is not clear in the rule as written.
- GFE Provider Burden as Related to Future Rulemaking on AEOB
The concerns outlined above on about the GFE for the uninsured or self-pay are even more important considering how they might relate to the GFE needed to initiate the AEOB. We urge the CMS to move away from the concept of a convening provider or facility when eventually implementing provisions related to the AEOB. It is unnecessary and extremely difficult to put one single provider in charge of collecting cost estimates, particularly when insurers will have all of the relevant information needed to generate the AEOB. If \a required step is implemented for
the AEOB where co-providers are required to send cost estimates to a convening provider before they go to the plan (instead of that information being sent directly to the plan), it has the potential to significantly delay care.
- Patient-Provider Dispute Resolution Process
The IFR established a patient-provider dispute resolution process, accessed when charges to an uninsured or self-pay patient are substantially in excess of the GFE—“substantially in excess” is
defined as at least $400 more than the GFE. We appreciate and support the patient protections established with this provision (for example, that a patient’s bill can’t be moved to collections while a dispute is pending). However, we urge CMS to consider revising the threshold for entering the dispute resolution process from $400 to a percentage of care in excess of the GFE instead. A threshold example to consider could be 15% more than the GFE. This type of system would require less adjustment over time as costs change. We also urge the CMS to consider a requirement that the disputed GFE must be a GFE provided once care
is scheduled—this reflects the concern that some information is not available before care is scheduled and the GFE may be more accurate once the care is scheduled.
As always, the Massachusetts Medical Society appreciates the opportunity to provide comments and work with CMS on our shared goal of providing the highest quality health care to patients. The MMS’ comments and recommendations are guided by our policies,
our membership, and our commitment to providing quality, equitable care to all patients. Should you have any questions, please contact Alexandria Icenhower, Federal Relations Manager, at aicenhower@mms.org or 781-434-7215.
\
Appendix A