Annual Oration 1975
By Harriet L. Hardy, M.D.
The friendly confidence of the Society in inviting me before and after a surgical operation on my head to fill this time-honored and privileged post has given me pause indeed. What is fresh and important that can be distilled from forty years of a varied and satisfactory medical career that will prove stimulating or helpful to physicians?
Drawing on 30 years of clinical study and care of patients with real or suspected job-related illness, I describe here some observations of risks taken daily by many workers and the responsibility of his doctor if a worker acquires disease that is occupational. In New England industrial risks are associated with the manufacture of storage batteries using lead, shipyard work, insulation in new and old construction, textiles and shoes, the use of beryllium in alloys and, until the early 1950's, phosphors for fluorescent lighting. In addition, a variety of potentially toxic materials are used in electronic and plastic industries.
All such activities have caused a remarkable number of clinical syndromes, few of which are exceptional enough to be immediately recognized. Beryllium disease mimics tuberculosis and Boeck's sarcoid, lead colic has led to unnecessary operation (occasionally prevented by a medical student's last-minute report of stippled cells in the smear of the patient's peripheral blood), and the pulmonary fibrosis of asbestosis has been pronounced idiopathic and the bronchogenic cancer of the asbestos worker considered due to cigarette smoking. Occasionally, and in contrast, such dramatic industrial epidemics as the recently documented angiosarcomas of the liver in the plastic industry and the mesothiliomas spawned in World War II by the increased use of South African crocidolite, a geographically separate form of asbestosis, widely publicized by the media, present quite different problems. Such advertisement as these two diseases have received has caused overdiagnosis, anxiety, fear of death and quick resort to litigation among exposed asymptomatic workers.
Who, in society, if not his doctor, is responsible for discovering the cause of job-related diseases, and initiating steps for job control of the hazard, and arranging for the patient-worker's medical care under the pitifully inadequate compensation laws now in existence?
Dr. Alice Hamilton, my late distinguished colleague, from her knowledge of earlier work in industrial disease, developed first by her study abroad in the latter half of the 19th century (and her first-hand sight of industrial disease in the United States), raised similar questions in the early 20th century. Knowing and working with her, learning our nearly identical personal reactions to industrial disease, I believe that in time, medically trained women in the United States will replace men as occupational physicians because of women's traditional urge to help the underdog. It may be true that most women are less impressed by the grand offices, presents of shares of stock in the companies, demands of the personnel manager or demands of company officials for the use of supposedly confidential medical files — facts of life today in many large industrial medical departments. Or, perhaps, in time, women would fall like Eve to some corrupting influence.
Joking aside, it should be understood that basic change to prevent occupational illness in the United States is coming as a result of strong pressures such as workers' active protest, progressive union leadership and the strength of a few brave activists in federal and state agencies; medicine should provide another pressure from an objective stance.
The federal laws of 1970 provided for the National Institute for Occupational Safety and Health (called NIOSH), for research and development of safe working standards, and the Occupational Safety and Health Administration (called OSHA), with the duty of enforcement. Such actions will affect physicians, especially those working part or full time in industry, since the law includes government access to workers' medical records.
What is the responsibility of the doctor for harmful results of worker risk? The history of this subject is not kind to doctors. There are shocking and true tales of women and young children working in coal mines, dragging carts of coal up steep slopes in the early years of the Industrial Revolution (Fig. 1). Lord Shaftesbury, a socially conscious peer of the realm, was able to put a stop to this practice in the United Kingdom in 1846 by powerful legislation. It is pitiful to report that in 1958 I saw a similar picture in a South American mercury mine: a child of 11 years hard at work.
The evils of young, ill fed children made to work as chimney sweeps among other menial jobs, the pay being used by their elders for gin, are well and movingly told by Blake, Dickens and Charles Kingsley in "The Water Babies" (Fig. 2). The only mention of a doctor in these 19th-century social horror stories is Sir Percival Potts, who described the scrotal cancer of Tom the Chimney Sweep, whose dirty clothes were saturated with carcinogenic hydrocarbons. No mention is made of therapy or prevention.
..jpg)
Figure 1: Children
Hauling Trucks of Coal, and Women Harnessed to Coal Trucks (Reproduced from
Hunter with the Permission of the Publisher).
..jpg)
Figure 2: Tom, the
Climbing Boy, in The Water Babies (Reproduced from Hunter with the Permission
of the Publisher).
In the United States, girls tipped their brushes filled with radium solution with their lips for the fine work of painting dials of airplane panels or watches. In the early 1920's, a pathologist, Dr. Harrison Martland, because he recognized their fatal anemia and sarcoma of bone as due to their jobs, and because he was unable to get care for these girls, enlisted the help of the local newspapers (Fig. 3). After a cartoon showing a death's head offering a dish of radium solution to a girl putting her brush in her mouth, widespread public sentiment came to Dr. Martland's aid.
In the early 1940's the disease at first called Salem sarcoid appeared in Massachusetts (Fig. 4). It is now known as beryllium disease, with 857 cases, a 26 per cent mortality and no recovery, on file with the Beryllium Case Registry. It is true and frightening to learn that physicians of the industry and the insurance carriers have fought the recognition and compensation claims of these patients through the years.
In my opinion, the responsibility for lack of interest and skill in occupational medicine lies with the medical schools and teaching hospitals. With rare exceptions, students are not taught how to take an occupational history or the rudiments of established knowledge of clinical entities associated with industrial hazards. For example, in the Department of Preventive Medicine at Harvard Medical School in 1949, I was responsible for 12 periods of teaching occupational medicine, and in 1971, for one 45-minute period. Some of us excited by this field have forced our way onto hospital wards with and without the invitation of the chief of service because of the value of discussing the work experience such as that of the patient with aplastic anemia due to inhalation of benzene — much more impressive than one sentence in a lecture. Thus, young, well trained doctors do not visualize occupational medicine as a career.
Few practitioners know that they must tell the patient, as soon as it is certain, that his illness is occupational. Next, they must instruct the patient to write at once to the company (keeping a copy) reporting his illness. If he does not do so, the company may be able to avoid liability. Few doctors realize how little money support present compensation laws give the sick worker, but of importance is the fact that in some states, including Massachusetts, the law does require the insurer to pay medical costs. The patient must pick his lawyer, who is paid nothing unless the patient wins. The company's lawyers, paid no matter what the decision, take refuge in delay and adversary-questioning technics, which successfully drive doctors from wanting to participate. Appointments to the Industrial Accident Board are made by the Governor, without required professional background, and its members may operate without trained advice unless they choose to engage a consultant or ask other agencies of the Department of Labor who are studying and controlling worker risk under state laws. A hardship for the sick worker is the fact that all third-party medical insurers, including Blue Cross/Blue Shield, will pay nothing when a worker's compensation claim is pending; nor will a hospital admit such a worker without a letter from an insurer willing to accept the cost (several of my patients have suffered delays of as long as 15 years). The economic rewards if the worker does win his claim are in most cases pitifully little; compensation benefits have been successfully kept low by insurance and employer lobbies.
Figure 3: Death and
the Girls Who Tipped Their Lips with Radium-Solution-Filled Brushes (Reproduced
from Hunter with the Permission of the Publisher).
..jpg)
Figure 4: Appearance
of a Patient with "Salem Sarcoid" (Beryllium Disease).
It is possible that the federal laws passed in 1970 (just now becoming operative) dealing with worker health will bring about some of the changes badly needed. This statement serves to introduce the subject of control of toxic exposures and the doctor's role in prevention of industrial disease. Fundamental is the fact that the physician alone cannot diagnose all cases of occupational illness or always know what resources he may use to keep his patient and other workers free from harmful job exposures.
Table 1 sets forth the duties of a team of various professionals needed for diagnosis of occupational diseases and, more importantly, for prevention. The military, the Atomic Energy Commission, some big industries, a few unions, insurance companies, various schools of public health, federal and state agencies are manned with such skills. The skills shown are those of professional chemical engineers or physicists who have chosen the field of prevention of harmful effect of potential hazards. The chemist and engineer are entitled industrial hygienists, the physicist, a radiation protection officer.
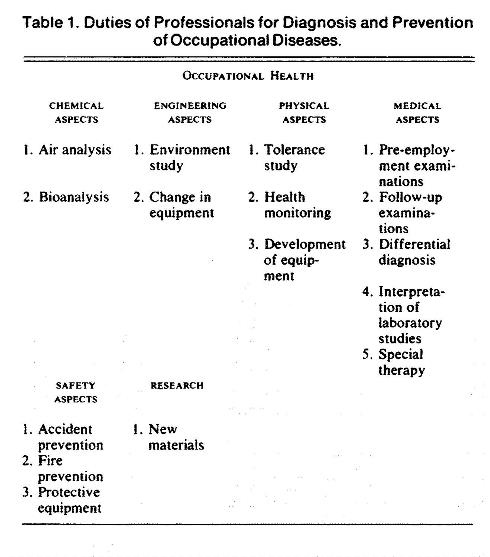
Table 1: Duties of
Professionals for Diagnosis and Prevention of Occupational Diseases.
In summary, workers in Massachusetts, New England and many parts of the world suffer needlessly from manmade industrial illness. A large body of knowledge available for proper diagnosis and prevention exists. Compensation claim processes are badly conceived and badly operated, to the hurt of the worker and to the financial well-being of the insurance companies. One can conclude that the medical profession must share blame for this state of affairs.
During the remaining time I want to discuss the risk of becoming a patient and some of the responsibility that the doctor assumes. The experience of my own two major medical events, both requiring operations and both with preoperative diagnoses of fatal disease, together with general and specialized medical practice since 1934, gives some authority to my opinions.
To weave a background for what I want to say, I have skimmed through several volumes of medical history and reread in some detail Dr. Howard Means's 1953 book Doctors, People & Government a series of Sir William Osler's essays, the early chapters of the Art of Treatment by W.R. Houston, and The Art of Ministering to the Sick by Richard Cabot and Russell Dicks.
In addition, I have read as much as possible in current medical literature of the pressure of current movements for change stimulated by government, organized medicine, medical groups, individuals, commissions variously appointed, leaders of unions, and officials of industries, as well as various insurance-company offerings for health care. One is bewildered by the welter of opinions and complex state of medicine at present. It is likely this audience knows more than I of the current evolution in the profession.
To turn, perhaps in simplistic terms, to some of the risks patients take in seeking medical aid, there are valid criticisms in my judgment. Worth repeating is the fact that competent medical advice and care are not widely available to either rich or poor. An important reason is that the profession has not seen fit to deprive ill trained and dangerous members of their right to practice. Although my example is not recent, the facts are true, and I doubt if they are unique. While studying the epidemiology of infectious hepatitis, I chanced on a privately owned hospital where I was shown a ward full of patients, some jaundiced, all of whom had laparotomy scars, and most of whom clearly had infectious hepatitis. Small wonder accreditation of hospitals is desperately needed. Furthermore, because I was working for the government at the time, I reported this experience to the Board of Registration in Medicine. I was told that the doctor responsible had had to take the examination five times before he was licensed to practice. Where was the County Medical Society on Ethics and Discipline? Why does the Board of Registration in Medicine not act to withhold the privilege of practice to such a poorly trained man?
Other reasons for the uneven quality of medical care are to be found in problems since World War II such as increase in demand for medical care, perhaps owing to an increase in real wealth, a slump in student interest in a medical career, and the spotty distribution of well trained practitioners in the United States. For how much of the present predicament is organized medicine to blame? A great variety of voices are speaking to these questions by word and deed. One must not underestimate the responsibility thoughtfully undertaken and wisely carried out by many practitioners in assessing criticisms and searching for changes.
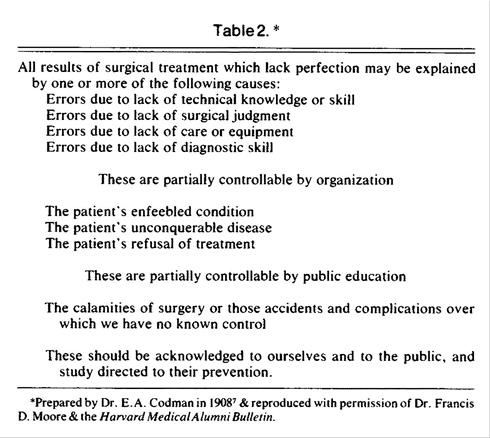
A further risk to patients is the decreasing willingness or ability (or both) of the family doctor to treat. Since World War II, greater and greater numbers of physicians are concentrating on less and less in their chosen field of medicine. The apology is, of course, the discovery of new technics and new knowledge. One wonders when the boards, societies, academies, colleges, and associations, most of them with subspecialties will stop multiplying, for the value of such certification becomes obviously misleading. There are new methods of testing the practitioner's ability to care for the sick under study and trial. One hopes a suitable course of action comes soon. I was much impressed with Dr. Francis D. Moore's essay on Dr. Amory Codman and Dr. Walter Cannon discussing the theme of technology and therapy and delivered to the Boston Surgical Society on November 5, 1973, when he received the Henry Jacob Bigelow Medal. Dr. Moore used this table prepared by Dr. E. Amory Codman (Table 2) as he told of Codman's struggle with hospital authorities to test scientifically the results of therapy. This table, which outlines Codman's plans, is dated 1908.
A quotation from Dr. Moore's 1973 essay seems to me appropriate in assessment of therapy (Codman had died 70 years earlier). "Modern intensive care in surgery has become a most elaborate matrix of interactions, electronic devices, and operative procedures...the opportunities for error have been multiplied a thousand-fold. Every patient that emerges from intensive care does so despite many misadventures." I add a plea for greater technical skill and sympathy for the patient during some of the modern diagnostic and therapeutic maneuvers which are painful and frightening. Although I know something of modern methods of reviewing treatment, does the profession correlate clinical events and therapy with outcome as keenly as Codman did and act to protect the next patient from this damaging drug or that ill conceived operation? Osler's words from his essay "Chauvinism in Medicine" underline our medical character leading in part to patients' risks: "No sin so easily besets us as a sense of self-satisfied superiority to others...it is an attitude of mind which leads to bigotry and prejudice or to such a vaunting conceit in the truth of one's own beliefs and positions, that there is no room for tolerance of ways and thoughts which are not as ours are."
A different subject is that of drug use. Diseases of Medical Progress, by Dr. Robert H. Moser, with an introduction by Dr. F. Dennette Adams, deserves careful reading. A useful saying taught me by a wise retired doctor comes to mind: "The well trained doctor knows what to do for his patient; the especially well trained doctor knows what not to do." The drug industry, in my experience, with rare exception, is a frightening, ever enlarging monster, sapping the physicians' judgment with spectacular advertisements and clouds of flattering samples. After an especially difficult talk with a clever drug drummer, I forbade my secretary to allow a drug salesman through my door again. The flow of samples diminished and then stopped. Surely, the patient must be protected from the risk and expense of many old and new drugs of potential harm to health and damage to financial resources. Osler discussed this problem in an address to the Canadian Medical Association in 1902 as follows:
The doctor's intellectual independence may keep the practitioner out of the clutches of the arch-enemy of his professional independence — the pernicious literature of our camp-followers, a literature increasing in bulk, in meretricious attractiveness, and in impudent audacity. To modern pharmacy we owe much...but the profession has no more insidious foe than the large pharmaceutical houses. We all know only too well the bastard literature which floods the mail, every page of which illustrates the truth of the axiom, the greater the ignorance the greater the dogmatism. Much of it is advertisements of nostrums foisted on the profession by men who trade on the innocent credulity of the regular physician....No class of men with which we have to deal illustrates more fully that greatest of ignorance which is the conceit that a man knows what he does not know.
Another risk to the patient and responsibility for the doctor is to be found in the fact that many consider the medical profession the most highly paid in society. A print of the so titled "Fashionable Physician" (Fig. 5), a drawing of the mid-19th century, was given me in the 1920's by my stepfather as part of a campaign to discourage me from undertaking a medical career. The line under the title reads; "He must have killed a great many people to get so rich...." It did not keep me from medicine, but it has always hung at eye level in my office. Is there a hungry doctor in the United States? I doubt it.
As a premedical adviser at M.I.T. in the 1960's, I posed a question to each student, "Are you planning to be a two-Cadillac-ambitious doctor?" —a question developed from a colleague's serious assurance to me that his tax man advised him that it was best to have more than one big car. Much of the talk at the doctors' lunch table in the past few years is of financial income and politics, and there are rarely discussions of interesting cases. This change calls to mind a comment made by the late Dr. Joseph Aub, a medical godfather of mine, when I quoted him the size of the bill sent by a colleague of both of us. "Oh" said Dr. Aub, "he has a cash-register mind." There is a vast distance between the 50-cent office call and the one-dollar house-call charge of my 1934–1939 practice geared to the Great Depression, and today's charges. You and I know there must be a change in today's medical economics. Perhaps Dr. Means's ideal of salaries for all doctors will prove the best way to keep a huge federal bureaucracy and litigation from our doors. I find it more than a little sad that the patient's ability to pay is no longer a criterion of the size of his bill. A farmer whose bill I had reduced because I knew he had had a poor crop, moved me almost to tears by saying: "Dr. Hardy, you have bowels of mercy." Organized medicine has much to do in this area and to blame insurance companies and the so-called recession is not reason enough.
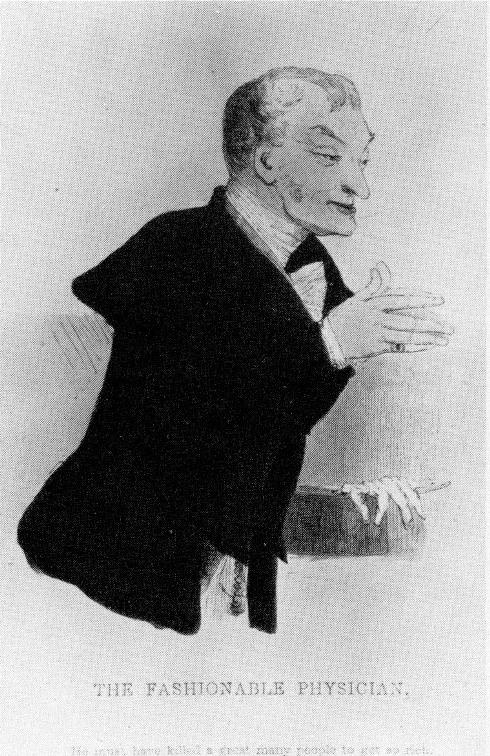
Figure 5: Nineteenth-Century
"Fashionable Physician."
Before stopping, I must plead for aggressive action in the field of confidentiality of patients' records. It is my view that patients should not be asked to sign all-inclusive, vaguely worded slips, freeing perhaps their innermost secrets, to an attractive clinical clerk for use in research or in court, for insurance claims, or in Social Security files. The Big Brother behavior by Washington revealed in the past few years applies to the use made of too many medical records. If action could be taken by organized medicine to correct this evil, it would go far to return the right to privacy of which we in the United States boast to the patient and ourselves.
Finally, what has been said here? What is its intent? It is not new. My reading has taught me that doctors have felt and acted as superiors to their fellows as long as there has been written history of medicine. Fénelon, a 17th-century French confidant and advisor to the great nobles of the court, wrote helpfully, "Are there not hypocrites in honesty to be found in the world, and ought we to conclude that there are no honest people because we find some false?" But as an observer for three years and activist for 38, my proud and noble profession looks to me to be sick at present. What are the causes? Two causes are obvious: the overpowering of the art of medicine by technology and the affluence of most doctors. The medical schools, too, share blame for the origin of the disease of our profession. They would do well to admit only students with evidence of humane standards toward others as well as themselves. Students should have had premedical studies in such fields as history and philosophy, political science and economics to help guide organized medicine from its narrow view of the world.
What is the cure? Repeated injections of humanity and compassion begun in premedical school years. Will the patient, our profession, recover? Yes, if the individual doctors and their organization can, with humility, accept the fact that much of the trouble that I have outlined and others not mentioned that you know of are the fault of "Chauvinism in Medicine," defined by Sir William Osler as "a narrow illiberal spirit in matters national, provincial, collegiate or personal."
This harsh indictment is relieved for me by my acquaintance and work with a number of thoughtful, forward looking physicians in Hanover and in Boston in the past few years. These doctors are clear headed and willing to work with and for our ill profession in and out of organizations. Their attitude makes certain a good prognosis.
_______________
Hardy, Harriet L. "Risk and Responsibility." New England Journal of Medicine 293, no. 16 (1975): 801-06.
View all Annual Orations
