By Sara Ruth Bates, MBE, Government Relations and Research Analyst
MMS advocacy for supervised injection facilities (SIFs) has reached the most important political arenas in the Commonwealth and the country. The Medical Society now serves as a go-to resource for legislators and policymakers who wonder what the state’s medical community’s position is on SIFs — spaces where people can inject drugs under clinical supervision and receive referrals to treatment and other services. Several key elected officials, including Boston Mayor Marty Walsh, have moved from skepticism to openness to exploring the establishment of SIFs in Massachusetts. How did we get here?
The Origin Story
The MMS’s work on SIFs began at the intersection of Albany Street and Massachusetts Avenue in Boston’s South End. It was the fall of 2015 and Nicholas Chiu’s first week at the Boston University School of Medicine (BUSM). Chiu had moved into a residence hall near the stretch of Mass. Ave. commonly called “methadone mile” for its abundance of methadone clinics and the prevalence of opioid use disorder (OUD) among the neighborhood’s denizens.
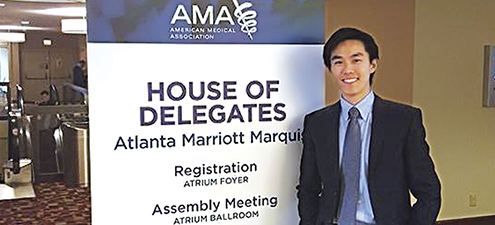
Nicholas Chiu at the 2015 AMA Interim Meeting where he got his first taste of health care activism. Photo by Sang Myung Han.
“Walking to school that first week, I remember seeing a number of people who were clearly struggling with opioid use. The most distinct memory I have was of one individual, clearly very sedated, stumbling into the intersection of Mass. Ave. and Albany. Cars were stopping abruptly and honking at him. At the time, it struck me as painfully ironic that so many people there clearly had OUD — and although they were in the vicinity of Boston Medical Center and Boston Health Care for the Homeless Program (BHCHP), they weren’t getting the care they needed. That was my first glimpse of the problem.”
Chiu then got a closer look at the human side of OUD. He took a two-year elective course, Homeless Health Immersion Experience, co-run by the BUSM and BHCHP. “We got to go into BHCHP and interview patients. We would talk with them for 40 minutes, sometimes even an hour, and they would open up to us about their lives. A large proportion of those patients were dealing with OUD. Through that
experience, I got a more personal look at people affected by opioids; it put a face on the problem.” But what could he do to help?
SIFs: An Evidence-Based Intervention
Chiu was only a first-year medical student, but he had a doctor’s mindset. “My first instinct was to look at the literature. I came from a research background, and I was used to doing systematic reviews of the literature and conducting meta-analyses.” He followed that instinct and learned about SIFs. “It shocked me how much literature there was on SIFs — over 100 studies. I started reading, and all of them showed reduction in opioid overdose deaths. None of the studies that I could find showed any deaths in a SIF. There were also increased rates of referral to addiction treatment, decreased rates of viral transmission, and no increase in crime.”
I thought, “This is clearly an evidence-based intervention that works. So many countries do it — so why doesn’t it exist in the United States? Reading more, I stumbled on the political and legal implications.” The data showed that SIFs saved lives, but political and legal impediments had blocked clinicians from establishing SIFs in the United States. Chiu was learning about clinical care, but he didn’t know how to get around political and legal roadblocks. “As a first-year medical student, I was curious about all those things, but I didn’t know at the time exactly what to do.”
With a Little Help from His Organized
Medicine Friends
Luckily, Chiu was very familiar with organized medicine and knew the support it could give medical students and residents. He chaired the MMS chapter at BUSM and had attended the MMS and AMA’s interim conferences. “I remember seeing medical students write resolutions. Those resolutions passed and influenced medical societies to take stances, and even advocate politically on specific topics.”
SIFs, he saw, would need political action to become a reality in Massachusetts. “I realized this was a very political issue, with complex legal implications. To actually move SIFs forward, it would not be enough just to create a buzz around the issue — you’d have to mobilize some sort of political action. My natural thought was, ‘What better way than the MMS
supporting this to move this issue forward?’”
Citing evidence from the literature, Chiu drafted a resolution for the MMS to advocate for a pilot safe injection site, then reached out to mentors at BHCHP and the MMS to connect him with other experts in the addiction medicine community to co-sponsor his resolution. “Through that process of working with MMS physicians and committees, I got a better sense of how this could really happen. When I first wrote the resolution, I had advocated for a much stronger stance — to start a pilot site in Massachusetts immediately. But after discussing the political climate with co-sponsors, we agreed to make some compromises in order to get this passed.” Tempering the proposal made sense from a scientific perspective as well — research on SIFs has been conducted outside the USA, “and the results are not necessarily generalizable to the US.” Chiu and his mentors agreed on a resolution that the MMS would first study the feasibility of SIFs and would then advocate based on the recommendations that emerged from their study.
From Idea to Resolution to Report and Beyond
The resolution passed, and the MMS Opioid Task Force researched and wrote a report on the feasibility of SIFs in Massachusetts that many legislators and policymakers have since utilized and cited. The MMS held a briefing on SIFs based on that report for US Senate staff in Washington, DC. The report was also shared with the entire Massachusetts congressional delegation. The MMS delegation to the American Medical Association (AMA) also brought a resolution on SIFs to the AMA’s House of Delegates, resulting in the AMA’s adoption of the MMS’s policy.
At the state level, the MMS successfully urged the passage of the first state SIF legislation in the country, requiring the state Executive Office of Health and Human Services to create a commission to study the feasibility of SIFs. MMS member Jessie Gaeta, MD, BHCHP’s chief medical officer, represents the Medical Society on the commission. At its latest meeting, she presented six of the strongest empirical studies on the efficacy of SIFs.
The MMS gave Chiu the mentoring and tools to make local and national change, as a first-year medical student. And Chiu has given the MMS the impetus to do what it does best: advocating for evidence-based policy interventions that can save the lives of patients, including Chiu’s former neighbors on Mass. Ave.
